Magnesium: A Key Player In Tissue Health, Inflammation, and Insulin Sensitivity
I have recently been focusing my research on the role dietary minerals play in maintaining health as I feel it is an overlooked aspect of nutrition. The last few weeks I keyed in on the role protein plays in calcium homeostasis and bone health and the potential dangers of high vitamin d and calcium supplementation. In this post I will be shifting my focus from calcium to another critical mineral, magnesium. We will look at the role magnesium plays on bone and soft tissue health, as well as the role magnesium plays in inflammation and insulin resistance .
An overview of Magnesium
Magnesium (Mg2+) is an atomic mineral involved in more than 300 essential metabolic reactions and plays an essential role in a wide range of fundamental biological processes. Magnesium plays a critical role in bioenergetics as ATP is bound to Mg2+, it is required for many of the key enzymes in glycolysis, the krebs cycle, and gluconeogenesis. Glutathione, our master intracellular antioxidant requires Mg2+ for synthesis (1). It plays a critical role gene transcription, activation, and regulation (2). While the list quite extensive, perhaps the most intriguing role for future research is the role Mg2+ has in cell signaling (3). I would love to discuss all of these roles, however for the sake brevity I will focus on bone and soft tissue health, inflammation, and insulin resistance.
Magnesium, bone, and soft tissue health.
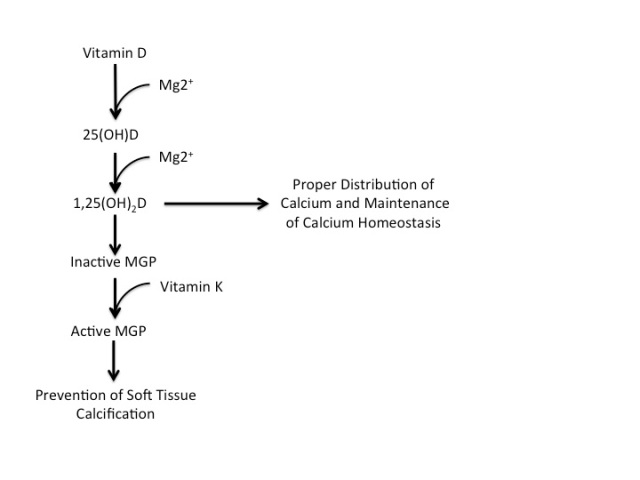
Magnesium plays a pivotal role in preventing soft tissue calcification. One of the main mechanisms through which magnesium prevents soft tissue calcification is the activation of vitamin D. As we discussed in the post last week, vitamin D produces MGP which is then carboxylated by Vitamin K2. Vitamin D in its initial form is considered “non-active” and requires activation in a two-step conversion process which requires Mg2+. This then allows vitamin D to produce MGP and also direct calcium to our bones (Figure 1).
Figure 1. Magnesium is required for conversion of inactive vitamin D to active vitamin D for the production of MGP and calcitriol and the proper distribution of calcium.
As I discussed in the post on protein and bone health, we maintain blood calcium levels through the hormones calcitonin and calcitriol (1,25 (OH)2D). This feedback look is rendered ineffective when we are deficient in Mg2+ as we cannot successfully activate vitamin D to calcitriol.
Recent research has shown that Mg2+ deficiency is associated with soft-tissue (vascular) calcification and that higher Mg2+ prevents calcification and the further progression of already established calcification (4). Additionally, there is evidence that Mg2+ supplementation reduces bone turnover, theoretically indicating improved bone density in post-menopausal women (5).
Magnesium Deficiency and Inflammation
In addition to the role Mg2+ in promoting health bone and soft tissue, Mg2+deficiency has been associated with type 2 diabetes (5), cancer (6), and cardiovascular disease(7). While there is insufficient evidence to pinpoint a causal mechanism, the current hypothesis is that Mg2+deficiency can result in inflammation. In fact, most pathological conditions associated with Mg2+deficiency occur due to chronic inflammation (8,9).
One of the most compelling pieces of evidence implicating Mg2+deficiency as a causal factor in inflammation was a study conducted over 75 years ago. This paper (10) written by Cruse et al. clearly highlights the importance of magnesium and its role in inflammation. While Cruse and colleagues were unable to explain how Mg2+ deficiency influences inflammation, recent research has in fact shown one potential mechanism, specifically related to heart disease. Maier et al. (11) successfully demonstrated that Mg2+ deficiency activates an inflammatory response and elevates the concentration of circulating cytokines in rodents (Figure 2).
Figure 2. From “Low magnesium promotes endothelial cell dysfunction: Implications for atherosclerosis, inflammation and thrombosis” by Maier et al. (2004)
The results of their study also found increased markers of cell adhesion, indicating a more atherogenic environment. The author’s concluded their study stating “Our data show that low magnesium directly affects endothelial cells, therefore indicating that the endothelial dysfunction caused by low Mg can contribute to generate a pro-inflammatory, pro-thrombotic and pro-atherogenic environment leading to cardiovascular disease.
According to Maier et al., low Mg2+ promotes an inflammatory environment and results in an increased atherogenic environment. This begs the question, will increasing Mg2+ help decrease inflammation. To answer this question we look to research published in 2007 by Scanlan et al (12) and 2012 by Sugimoto et al (13).
In 2007, Scanlan used a rat model to examine the effects of Mg2+ deficiency on gut health and inflammation. The results of this study demonstrated that a Mg2+ deficient diet alone induced a proinflammatory state in the gut. The effect of this Mg2+ deficiency induced inflammation was not confined to the gut, it was systemic. They observed a reduction in blood glutathione, confirming that it induced systemic oxidative stress. The data indicate that gradual development of Mg2+ deficiency induces subclinical inflammation, and that acute magnesium repletion attenuated the exaggerated inflammation.
The work by Sugimoto et al. was able to provide even more detail on the mechanism through which Mg2+ deficiency induces inflammation. Sugimoto et al examined the effect MgSO4 had on biomarkers of inflammation (TNF-α and IL-6) as well as NF-kB, a protein that controls DNA transcription involved in inflammation and immune response. Their study showed MgSO4, specifically the magnesium component decreased TNF- α and IL-6 production. By reducing NF-kB activation. From their findings, the authors concluded “Our results define a novel immunomodulatory function for MgSO4, whereby it regulates NF-kB activation, cytokine production, and limits systemic inflammation.”
Taken together, the body of evidence suggests that magnesium deficiency plays an important role in the pathogenesis of inflammation. Additionally, while the degree to which magnesium deficiency plays a role in the development of inflammation it appears as though magnesium deficiency may indeed be a contributor causal role in the development of inflammation associated diseases such as diabetes and heart disease.
Insulin Sensitivity
It has been well established in the literature that inflammation plays a role in the pathogenesis of insulin resistance (14). The mechanisms through which inflammation induces insulin resistance is beyond the scope of this article, and the curious read can refer to reference 14. Magnesium can clearly play a role in the development of inflammation; therefore, magnesium may have an indirect effect on insulin sensitivity. Additionally, and probably more importantly, Mg2+ has a direct effect on glucose metabolism and insulin sensitivity.
Intracellular free Mg2+ concentrations are critical in the phosphorylation of the tyrosine–kinase of the insulin receptor (15). Phosophorylation of this tyrosine-kinase is critical in maintaining proper cell signaling and thus glucose metabolism.
Magnesium deficiency may result in disorders of tyrosine–kinase activity on the insulin receptor, ultimately decreasing glucose utilization (16). Therefore, lower basal Mg2+ requires a greater amount of insulin required to metabolize the same glucose load, resulting in decreased insulin sensitivity (Figure 3).
Figure 3. c/o John Libbey Eurotext
Taken together it appears that magnesium contributes to insulin resistance directly through decreased insulin-receptor tyrosine-kinase phosphorylation and indirectly through increased inflammation.
Clearly, there is an established mechanism indicating that Mg2+ deficiency can result in decreased insulin sensitivity. This begs the question; can correcting Mg2+ deficiency in those with already established insulin resistance improve insulin sensitivity? To answer this question I turn to research published in Diabetes Care in 2003.
In a randomized double-blind controlled trial, Rodriguez-Moran & Guerrero-Romero took 63 subjects with established type 2 diabetes and decreased serum magnesium and treated them with either MgCl2 or placebo for 16 weeks. The results of their study showed that correcting Mg2+ deficiency with MgCl2 increased serum magnesium and increased insulin sensitivity while decreasing fasting glucose and HbA1c. Essentially, this successfully demonstrated that Mg2+ supplementation in those with Mg2+ deficiency does in fact improve insulin sensitivity and metabolic control (17).
Natural Sources of Magnesium
Supplements can and should be used to correct deficiencies and the “right the ship”. However, I would argue that attempting to derive our necessary minerals from whole foods sources is a better practice as it promotes “nutrient synergy”. Many of the foods high in magnesium include whole grains, nuts, and seeds. However, the magnesium in these foods is not highly “bioavailable”. Magnesium is often bound up in other chemicals reduce its bioavailability including phytates and oxalates (18). Magnesium is also found in meat sources, which increases its absorption and bioavailability. Highly processed foods, including refined grains are essentially void of magnesium. This indicates that an evolutionary approach to nutrition that promotes meats, vegetables, nuts, seeds, some “safe” starch and fruit will help individuals maintain a healthy level of magnesium.
Summary
It is clear that magnesium is critical in maintaining life and our body’s capability to execute innumerable vital functions. Unfortunately, as research has currently shown, a vast majority of American’s fail to meet the daily requirement for magnesium (19). The evidence in this post suggests that magnesium Mg2+ deficiency may in fact be a key contributor to the declining health in America, and the rest of the world. In light of this evidence it would be pertinent to adopt an evolutionary approach to diet and nutrition in order to obtain sufficient levels of magnesium in order to promote bone health, prevent soft tissue calcification, maintain normal inflammation, and promote normal insulin signaling and function.


Greetings >>>>
Really enjoyed reading this post >>
I am currently studying to become a nutritional healer and am reading a book called the Magnesium Miracle…. Fascinating read
Love and light I-tinually